
The cervical space during your first pregnancy is not as elastic as it is for a woman who has already given birth. Women who have already experienced childbirth have a wider cervical canal than women experiencing their first pregnancy.

Some women don’t lose their mucus plug at all during pregnancy. The way a woman loses the mucus plug is different for women experiencing their first pregnancy than women who have already had children. The mucus plug is much thicker and more gelatinous than typical pregnancy discharge. There is an evident difference between normal discharge and the mucus plug.
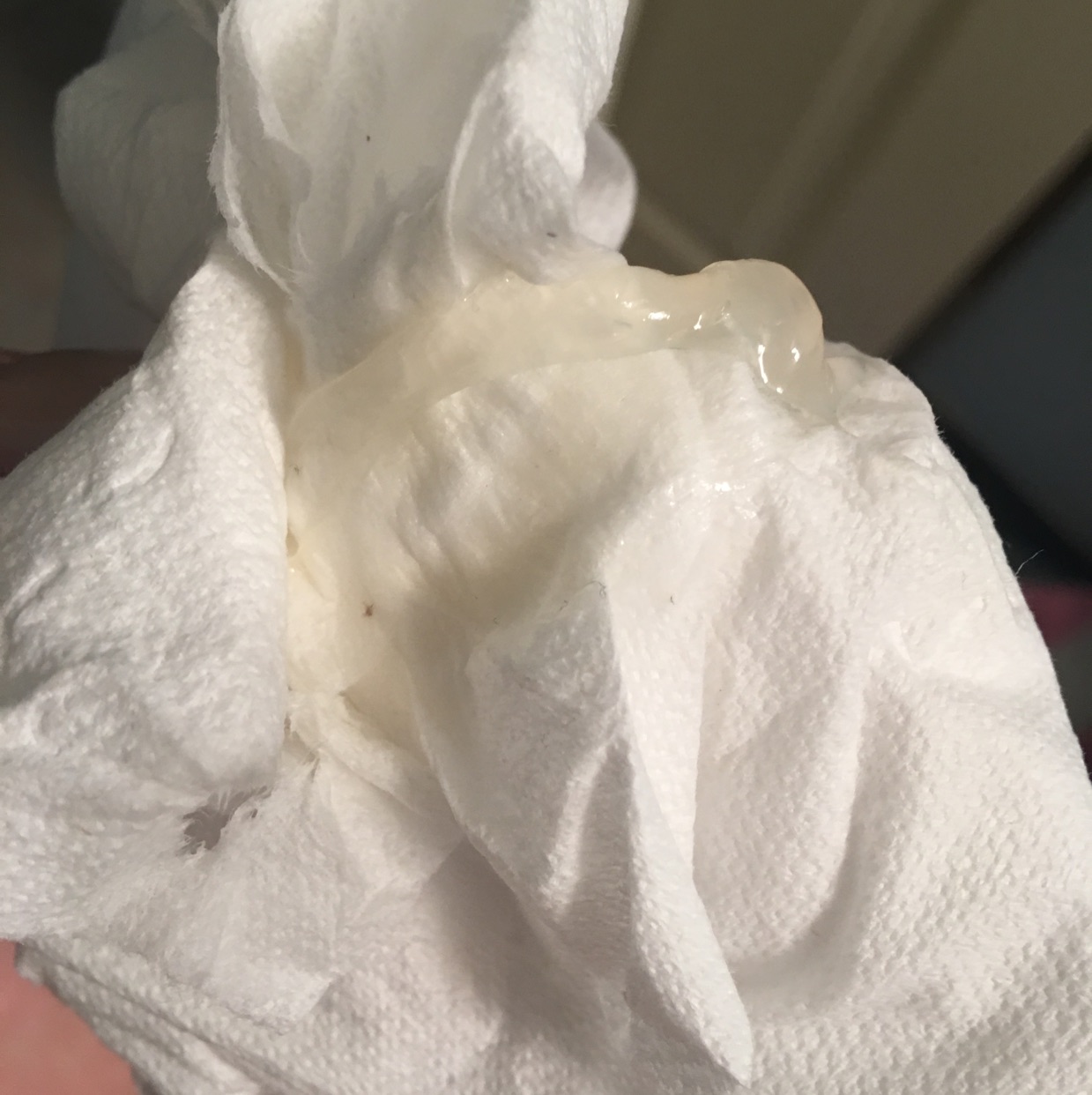
But some of the pictures might make you squeamish, so be prepared! If you are a visual person, you can look up numerous pictures on Google to give you an idea of what you should be looking for. You may notice red streaks within your mucus plug because as your uterus expands to release the plug, capillaries can burst, causing a minor amount of bleeding, leading to the streaking. The plug is usually about 4 to 5 centimeters long, but it is not unusual for your mucus plug to come out in pieces and not all at once. The plug is thick when in place, but it usually thins out and develops a liquidy texture when passing. The mucus plug kind of resembles boogers - not so classy, but it serves a purpose. Your mucus plug can vary in color, but it is typically clear, yellow, green, pink, white, or brown. Your mucus plug is not fully formed at this point - it increases in its consistency every month of your pregnancy. Your cervix softens around this time, which allows the area to become filled with the cervical mucus, creating a seal for the uterus. Your mucus plug begins forming when the ovum implants in the uterine cavity around the end of your first month of pregnancy. It will thicken each month until you are near delivery. It is a thick material with a similar texture to gelatin. commune and Aspergillus 3 was found to be difficult in previous cases, both species could be identified as filamentous fungus in our case.The mucus plug is formed by secretions from your cervical glands. 2 Although the morphological differentiation between S. When tests were performed using sputum-derived cultures obtained from 213 Japanese patients with ABPA/ABPM, Aspergillus species and Schizophyllum commune were identified in 126 (59%) and 12 (6%) patients, respectively. Further molecular tests were not available at our clinical site. 1 Although the morphology of the filamentous fungus was similar to that of Aspergillus, we were unable to confirm the species, as the culture result from the bronchial wash was not positive for any fungus. Mucoid impaction, a clinical radiographic syndrome manifested by inspissated mucus plugs of the bronchi, most commonly occurs in patients with inflammatory conditions such as allergic bronchopulmonary aspergillosis (ABPA)/mycosis (ABPM) however, as in this case, it is also observed in patients with benign and malignant conditions causing airway obstruction. This case revealed evidence of mucoid impaction associated with fungal infection in a patient with lung SCC. The patient was followed up without any complication 1 month after the surgery. Analysis of surgical specimens revealed SCC ( figure 2C, D) without any lymphatic or vessel involvements there were no evidence of eosinophilic inflammation and fungal infection. He underwent left upper lobe lobectomy to treat obstructive pneumonia which developed after SCC diagnosis. Transbronchial biopsy specimen of the tumour showed squamous cell carcinoma (SCC) of the lung. Pathological examination of the mucus plug revealed fungal filaments ( figure 2B). Bronchoscopy revealed a tumour obstructing the lingular bronchus with a thick mucus plug ( figure 2A). Serum tumour markers, including carcinoembryonic antigen, cytokeratin 19 fragments and pro-gastrin-releasing peptide, were within normal levels and were similar to the levels 8 months before admission. Laboratory examination revealed a total leucocyte count of 6.3x10 9/L (range: 3.5–8.5x10 9/L) with a total eosinophil percentage of 2.6% (range: 1%–6%), total serum IgE levels of 1370 IU/mL (range: <173 IU/mL), and Aspergillus fumigatus-specific IgE of <0.10 kUA/L (range: <0.35 kUA/L). Chest CT revealed a large mass in the lingular segment ( figure 1B). Eight months later, he was readmitted to our hospital due to deterioration of chest radiograph findings. Bronchoscopy was not performed as he refused further investigations owing to improvement in haemoptysis, and he was lost to follow-up. Chest CT showed mucoid impaction-like consolidation from the bronchus to the lingular segment but no lymphadenopathy ( figure 1A). He had no other symptoms, and physical examination was unremarkable. A 64-year-old healthy man with mild haemoptysis for a month was referred to our hospital.


 0 kommentar(er)
0 kommentar(er)
